Pathogenesis of Rhinoviruses Infection
C. Pathogenesis
The primary site of rhinovirus infection is in the nasal epithelium. Virus may be detected in the nasal washings of volunteers 24 hours after inoculation and reach a maximum peak by the second or third day. The titres then start to decline and the virus is usually undetectable by the fifth day. Symptoms of cold appears one day after inoculation and peak on the third or fourth day. It is uncertain whether rhinitis is due to the direct cytocidal effect of virus replication or through the release of mediators. Histamine have not been shown to play any role in the development of rhinitis. Kinins, however, are found in elevated quantities. Volunteers given kinins intranasally develop cold symptoms.
Following infection, a specific humoral response is found in
both serum and nasal secretions. Serum-neutralizing antibodies do
not appear until 14 days after infection and thus recovery is
probably not mediated by antibodies. Serum antibodies remain
elevated for many years and are probably responsible form
protecting the person against reinfection. However, local
neutralizing antibodies are lost after 2 years.
D. Clinical Symptoms
The common cold is characterized by rhinorrhoea, nasal obstruction, sneezing, sore throat and cough. There is little fever and systemic reactions are uncommon. The illness may last for a week or more. Otitis media and sinusitis may complicate rhinovirus infection in a small proportion of patients (<1%), usually in conjunction with a bacterial infection. The exact role of rhinoviruses in the development of otitis media is not clear. Rhinovirus infections also induce the onset of asthmatic attacks in atopic individuals. Very rarely, rhinovirus infections are associated with cough, chest pain, bronchiolitis and bronchopneumonia. The general opinion is that rhinoviruses are not a significant cause of croup, bronchiolitis , or viral pneumonia.
E. Laboratory Diagnosis
Usually, a common does not require laboratory investigation. If required, the diagnosis is generally made by the isolation of the virus in a sensitive cell culture. Nasal washings are the best specimens and should be collected early in the disease when maximal titres of virus is excreted.
F. Treatment_and_Prevention
Early attempts to prevent rhinovirus infections by vaccination have not been successful. The diversity of rhinovirus serotypes and the lack of cross-protection during reinfection with heterologus serotypes makes prevention by vaccination unlikely to succeed. Attention has therefore focused on the development of antiviral molecules such as interferons and synthetic anti- rhinovirus compounds which could be used therapeutically as well as prophylactically.
Prophylaxis - Natural and recombinant interferon have been shown to be effective in preventing both infection and illness when given intranasally in volunteers over short periods of time. However, prolonged administration resulted in considerable local cytotoxicity reactions eg. nasal irritation, ulceration and bleeding. It is clear that interferons can not be used for long periods, although they may considered for use over short periods eg. 1 week to prevent an infection within the family setting. Given this way, no side effects were reported in volunteers. A number of synthetic compounds have been developed which have potent anti-rhinovirus effects in vitro. One of these compounds, R61837 was shown to be effective in vivo when it significantly suppressed the appearance of colds in volunteers given this compound prophylactically.
Treatment - Clinical trials with interferons failed to modify the course of rhinovirus colds. A recent trial with R61837 again failed to modify the course of a clinical rhinovirus cold. Because of the multiplicity of serotypes, it would be very difficult to develop an effective vaccine against rhinoviruses. Therefore the pursuit of antiviral agents remains the best option.
Coronaviruses
Human coronaviruses were first isolated in the mid 1965 from volunteers at the Common Cold Unit. The coronaviridae are a monogeneric group of RNA-containing viruses that are associated with respiratory infections in animals, including pigs, cats, dogs, mice and chickens. The group was so named because of the crown-like projections on its surface. At present, at least 10 species are recognized, of which human coronavirus is one. The other are found in animals.
A. Properties
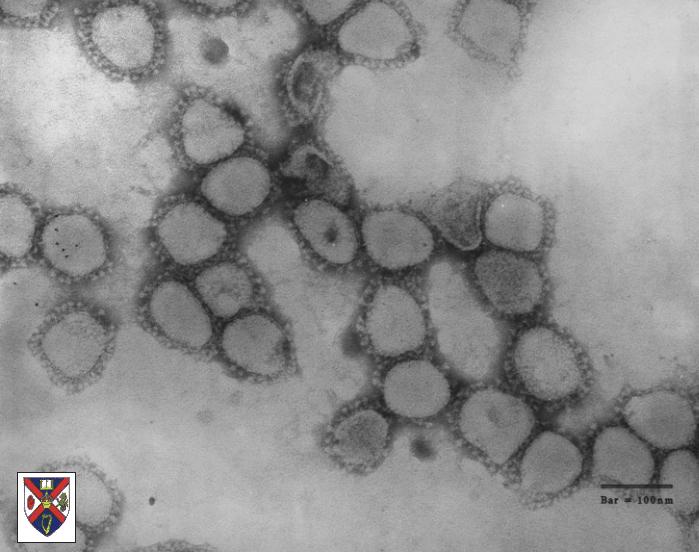
ssRNA enveloped viruses of pleomorphic morphology
60 to 220nm in diameter.
Positive stranded RNA; helical symmetry
characteristic club-shaped projections of 20nm, involved in neutralization, fusion and in some coronaviruses, haemagglutination.
Electronmicrograph of corona virus particles.
Some Human Coronavirus strains, namely 229E and serologically
related strains, are generally readily propagated in human cell
culture. However, other human coronavirus strains, namely OC43
and some serologically related strains, are considerably more
difficult to propagate in cell culture. Three antigenic molecules
are found in the virions ie. nucleocapsid, surface projection and
transmembrane proteins. The NP antigens may be common to all
coronaviruses, while the main antigenic determinants of
individual viruses reside on the surface projections. The surface
projection antigens are used for the serological grouping of
coronaviruses. One avian and two mammalian serological groups
have been established. Human coronavirus strains fall into each
of the mammalian groups which are named the OC43 and 229E
serological groups. It is not clear how closely related are the
viruses within a serological group.
B. Epidemiology
Generally, human coronavirus infections occur during the winter and early spring but the peak period may vary by several months. The periodicity of infections caused by 229E and OC43 group viruses follows a complex pattern, although they usually cycle with an interval of 2 or 3 years. In general, high infection rates in any particular year are caused by either 229E or OC43 group viruses with only the occasional sporadic human coronavirus infection belonging to the other group. This pattern is observed throughout the world.
C. Clinical Features
Human coronaviruses are responsible for 10 - 30% of all common colds. All age groups are affected, and infection rates have been shown to be uniform for all age groups. This is different from other respiratory viruses such as RSV, where there is a distinct decrease in infection rates with an increase in age. The incubation period is short, being 2 to 4 days. Infection may also be subclinical or very mild. There have been some reports of more severe lower respiratory tract involvement in young children and old people. Reinfection of individuals with the same human coronavirus serotype often occurs within 4 months of the first infection, suggesting that homologous antibodies are protective for only 4 months. Although many people have high antibody levels after infection, reinfection with the same or related strains is common. Antibodies to one human coronavirus group may not be protective against infection with viruses from another group. There are no differences in pathology observed between the OC43 and the 229E strains.
Other possible infections - coronavirus-like particles
are often seen in the faeces of children and adults suffering
from diarrhoea. These particles have a different morphological
appearance to those seen in respiratory infections. As yet, there
is no firm evidence associating the presence of these particles
to diarrhoea. Also human coronavirus particles have been observed
in tissue form patients suffering form multiple sclerosis, there
is no evidence for an aetiological role.
D. Diagnosis and Treatment
Diagnosis of human coronavirus infections is not attempted in many routine laboratories. They have fastidious growth requirement in cell culture, and the conditions caused by them are of minor clinical significance. The routine diagnostic procedures comprises of cell culture and serology.
Virus isolation - 229E and related strains can be isolated in roller culture monolayers of human embryonic lung fibroblasts, such as W138 and MRC5 cells. A virus CPE of small, round, granular cells is seen throughout the monolayer. Isolates can be confirmed by virus neutralization tests. OC43 related strains usually cannot be grown in cell cultures. Isolation has to be performed on organ cultures of human embryonic tissue such as trachea.
Serology - virus neutralization are the most frequently used tests. HI, CF and ELISA tests have been used. Most of these tests are not carried out in routine diagnostic laboratories. There is little, if any, antibody cross-reaction between strains of 229E and OC43.
Direct detection of virus - indirect immunofluorescence and ELISAs have been developed to detect the presence of coronavirus antigen in nasal secretions with differing results. The usefulness of indirect immunofluorescence has still to be established.
No antiviral drugs against coronaviruses are available and little research is being taken to produce any. However, vaccines against certain animal coronaviruses are available.