Laboratory Diagnosis of Herpes Simplex Viruses Infection
Laboratory Diagnosis
1. Light Microscopy - cells from the base of the lesion, or wiped from a mucous surface, or biopsy material, may reveal intranuclear inclusions (Lipschutz inclusion bodies). Infected cells may show ballooning and fusion.
2. Electron Microscopy - Electron microscopy is not a sensitive tool for the detection of HSV, except in the case of vesicle fluids which often contain 108 or more particles per millilitre. However, like light microscopy, electron microscopy cannot distinguish between the different viruses.
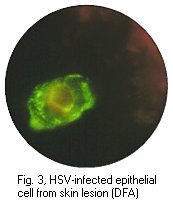
3. Direct examination by antigen detection - cells from
specimens are treated in ice-cold acetone. FITC is generally used
for staining of fixed material. It is more sensitive and specific
than light and electron microscopy (90% sensitive, 90% specific),
but cannot match virus culture. In terms of cost and technical
expertise, it is very much more demanding.
 |
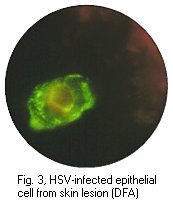 |
Cytopathic effect of HSV in cell culture, note the balooning of cells (Courtesy of Linda Stannard, University of Cape Town, S.A.) and positive immunofluorescence test for HSV antigen in epithelial cell (Virology Laboratory, Yale-New Haven Hospital)
4. Virus Culture - infectious HSV-1 and HSV-2 are amongst the easiest viruses to cultivate. The fresher the lesion, the better the chance for recovery, ulcers and mucous membranes should be swabbed as vigorously as possible. Virus transport medium should be used but this is not critical provided that desiccation is avoided. Saliva, urine, CSF and biopsy material do not need transport medium. Inoculation should be carried out as soon as possible. A wide range of cell lines are available for isolation. At least 2 cell lines should be chosen. A typical CPE may appear from day 1 onwards. Other viruses can occasionally mimic the CPE of HSV. Formal identification of the isolate can be carried out by immunofluorescence, complement fixation, neutralization or electron microscopy.
5. Serology - CFTs are commonly used, as are indirect haemagglutination (IFT) assays which are more sensitive than CFTs. Weak antigenic cross reaction with VZV may occasionally cause problems in these tests. ELISAs and RIAs are becoming available and may gradually replace CFTs and IFTs. Seroconversion from a zero baseline is usually diagnostic of a primary infection. In the case of recurrent infection, an immune response from a non-zero baseline may be detected. For immune status screen, sensitive tests such as ELISAs and RIAs should be used as insensitive tests such as CFTs may fail to detect very low levels of HSV specific antibodies which are present years after a primary infection.
In contrast to many other viruses, HSV specific IgM had proved to be unhelpful in the diagnosis of primary infection as HSV IgM may be present in cases of reactivation as well as primary infection. In certain circumstances, HSV IgM may be useful in the case of neonates when the presence of HSV IgM is a highly significant finding, as can be its detection in the CSF of a patient with suspected encephalitis.
Herpes_simplex_encephalitis ;- The diagnosis of HSE is difficult, therapy should be commenced as soon as possible where there is suspicion of HSE on clinical grounds before the results of laboratory tests are known. HSE cannot be diagnosed reliably by virus isolation from the CSF or by IF using CSF cells. HSE is diagnosed by the following methods;-
(a) HSV antigen by FITC conjugated anti-HSV antibodies from brain biopsy cells.
(b) Virus culture from brain biopsy cells
(c) The presence of HSV virions or Lipschutz inclusion bodies in brain tissue by electron or light microscopy.
(d) The demonstration of intrathecal synthesis of HSV antibody.
Brain biopsy provides the best avenue for diagnosis but is
rarely carried out nowadays with the advent of acyclovir. For
determination of intrathecal HSV Ab synthesis, the integrity of
the blood-brain barrier should be assessed to ensue that any HSV
Ab present in the CSF is not a result of transudation from the
serum across a compromised blood-brain barrier to the CSF, as is
the case during the early stages of acute necrotizing
encephalitis.
Management
A._General_Management
Steriods have little place in the management of HSV infections as they tend to exacerbate the situation through their immunosuppressive effect. Every effort should be made to reduce the dosage of steroids where herpes simplex develops in a person receiving high dosage steroids eg. eczema, rheumatoid arthritis, graft surgery etc. Steroids are only indicated in cases of severe stromal herpes or erythema multiforme where hypersensitivity is an important part of the pathogenesis. The general management of severe mucocutaneous HSV infections include supportive procedures, analgesia and antibiotic treatment of secondary bacterial or candida infections.
B._Antiviral_chemotherapy
At present, there are only a few indications of antiviral chemotherapy, with the high cost of antiviral drugs being a main consideration. Generally, antiviral chemotherapy is indicated where the primary infection is especially severe, where there is dissemination and when sight is threatened. Urgent treatment is required in the face of a life-threatening HSV infection in the eczematous or immunocompromised patient, in the neonate, in HSE, and in patients with eczema herpeticum. It is not necessary to treat HSV disease if it is not sufficiently severe to warrant hospital admission. Exceptions to the rule include painful herpetic whitlows and all forms of ocular herpes. Recurrent disease other than ocular disease in normal individuals rarely merits specific chemotherapy.
Specific anti-HSV drugs are more effective in the treatment of primary infection and should be given within 3 days of the onset of symptoms. They are rarely effective if given more than 5 days after the onset of symptoms. With recurrent disease, treatment must be initiated in the prodromal phase before the appearance of symptoms or treatment will prove to be valueless. The following are anti-HSV drugs currently used in the UK.
1. Acyclovir - This is the drug of choice for most situations at present. Acyclovir require the presence of a HSV-encoded thymidine kinase in order to be converted into its active acyclovir triphosphate form. Acyclovir triphosphate is a potent selective inhibitor of HSV DNA polymerase and causes premature chain termination when it competes with guanine triphosphate for incorporation into newly synthesized viral DNA. Acyclovir is available in 4 formulations (in parentheses, licensed uses in the UK):
1. i.v. (HSV infection in normal and immunocompromised patients)
2. oral (treatment and long term suppression of mucocutaneous herpes and prophylaxis of HSV in immunocompromised patients)
3. cream (HSV infection of the skin and mucous membranes)
4. ophthalmic ointment
Acyclovir has few mild side effects and is generally very safe to use. After prolonged high doses, acyclovir can cause bone marrow depression but this is not likely to be encountered in normal clinical practice. Acyclovir resistant strains of HSV have been reported. These resistant strains fall into 3 categories:
1. Naturally occuring thymidine kinase negative variants
2. Thymidine kinase resistant mutants (Tk-)
3. pol mutants with a DNA polymerase resistant to inhibition by acyclovir triphosphate.
Only Tk- variants have emerged in nature following the therapeutic use of acyclovir. However, both types of mutants are associated with reduced pathogenicity. Forscarnet and ara-A are the drugs of choice for the treatment of acyclovir resistant HSV.
2. Famciclovir - famciclovir is the prodrug of penciclovir which is the active form and a guanosine analog. It has a very high bioavailabiity of 77%. It is converted into penciclovir by a two step process. The first step occurs in the gut and the second step in the liver. It has a long half life in the gut. It has a higher affinity for HSV thymidine kinase than acyclovir but a lower affinity for HSV DNA polymerase than acyclovir. It acts as an inhibitor of viral DNA polymerase and also as a chain terminator. It is used for the treatment of primary and recurrent genital herpes, and for long term suppression of recurrent genital herpes.
3. Valaciclovir - valiciclovir is the prodrug of
acyclovir but is much more readily absorbed by the gut than
acyclovir. It is used for the treatment of primary and
recurrent genital herpes, and for long term suppression of
recurrent genital herpes.
4. Idoxuridine and trifluorothymidine - idoxuridine is highly toxic when given systemically and is now only used in the eye. trifluorothymidine is an excellent drug in ophthalmic practice but it does not have a product license and is only available on a named patient basis in the UK.
5. Vidarabine (ara-A) - intravenous ara-A can be used for the treatment of neonatal herpes and HSE. It is not available as an oral preparation but can be used topically in the treatment of ocular infections. Ara-A does not have a product license for use in the UK for treatment of HSV infections.
Acyclovir has all but replaced ara-A for systemic therapy. This shift is not necessarily soundly based as there is little evidence that acyclovir is more effective than ara-A when used systemically. However, there is no doubt that ara-A is a much more toxic compound than acyclovir as it can cause bone marrow depression and its use should be monitored by regular full blood counts. Topical therapy for mucocutaneous herpes is probably of minimal benefit outside ophthalmic practice. Idoxuridine and acyclovir cream are available for the treatment of oral or genital herpes but are of doubtful value.
Prophylactic_antiviral_chemotherapy
Prophylactic anti-HSV chemotherapy may be indicated in the following situations ;-
1. Bone marrow graft recipients - BM graft recipients become intensely immunodeficient and HSV is an important cause of post- transplant morbidity and death. Generally, acyclovir is given as maintenance prophylaxis for 6 to 9 months, beginning 3 days before transplantation.
2. Patients who suffer frequent recurrences of oral or genital herpes - A daily dose of acyclovir 800mg (1000 mg during immunosuppression) will have a favorable effect on recurrences. The current cost is over £1000 per annum though. The response is better for herpes genitalis than labialis lesions.
Herpes_Simplex_Encephalitis
It is still unclear whether the prognosis of HSE is affected to a great extent by specific chemotherapy. The outcome in HSE is dependent to a great extent on the quality of the general medical care. Patients die from this disease because of the unremitting cerebral oedema and damage to critical neurological systems. The cerebral oedema should be aggressively controlled by dexamethasone, osmotherapy (urea, mannitol, or glycerol), hyperventilation, elevation of the head of the bed and if indicated, by surgical decompression. Acyclovir is now the drug of choice for the treatment of HSE. With the best treatment, the mortality of HSE can be reduced from 70% to 30%. Ideally, brain biopsy should be performed before specific antiviral chemotherapy is given but there is at present, a great reluctance to perform brain biopsy.
Ocular_Herpes
The management of ocular herpes is a highly specialized subject. In general, topical steroids must never be prescribed in any condition of the eye which carries the slightest suspicion of being ocular herpes. Surgical cleansing of the cornea (debridement) makes a significant contribution to healing and complements local antiviral chemotherapy. Secondary bacterial infection should be treated by antibiotics. There is a wide choice of anti- HSV preparations available and selection is difficult and mostly reflects personal preferences. A liberal amount of ointment should be used 5 to 6 times a day. Steroids are harmful and are strongly contraindicated in many forms of ocular herpes. When inadvertently used, dendritic and conjunctival ulcers fail to heal and spread to form large corneal ulcers which may perforate. The only situation when steroids are indicated are in the treatment of ocular herpes of the internal eye.
Prevention
On the whole, preventive measures against HSV infection have been disappointing. The virus is ubiquitous and little or nothing can be done to prevent the transmission of infection in environmental terms. HNIG has not been effective in the prevention of HSV infections. Prophylactic chemotherapy may be given to those suffering from frequent and severe recurrent herpes but the cost factor must be taken into account. In clinical trials, a -interferon eye drops have proved effective for the prevention of recurrent dendritic ulcers.
The only area where there has been some success is the prevention of transmission of infection to newborn babies by the use of caesarean section. The actual decision of whether to carry out a caesarean section or not is very difficult as maternal genital herpes is common whereas neonatal herpes is rare. Furthermore, asymptomatic shedding of HSV is common. Generally, caesarean sections are not carried out for cases of recurrent herpes (except where florrid lesions are present and with the mother’s informed consent) but for cases where there is florid primary infection. The neonate should be closely monitored and acyclovir should be given on the merest suspicion of genital herpes. If the mother develops primary HSV infection during the first or second trimester of pregnancy, antiviral therapy may be considered. If the mother contracts primary herpes during weeks 30-34 of pregnancy, she may be treated by a acyclovir followed by Casarean section or normal delivery. The mother with primary genital herpes between week 34 and term should be delivered by Caesarean section. A woman who presents with primary genital herpes while in labour may be treated with IV acyclovir, although it is uncertain whether this will reduce the rate of transmission.
HSV_vaccines - Several
recombinant subunit vaccines are being evaluated at present.
There is evidence to suggest that such vaccines may be effective
in reducing the frequency and severity of recurrent disease in an
already immune individual, but their efficacy in preventing
primary infection is uncertain. Primary infection per se is not a
condition worth preventing except in immunosuppressed patients.
However, such vaccines may be useful in preventing or attenuating
recurrent disease.