DELTA_AGENT
The delta agent is a defective virus which shows similarities
with the viroids in plants. The agent consists of a particle 35
nm in diameter consisting of the delta antigen surrounded by an
outer coat of HBsAg. The genome of the virus is very small and
consists of a single-stranded RNA. Eight genotypes (HDV-1 to -8) and several
subgenotypes have been described. There is a worldwide
distribution of hepatitis D in association with hepatitis B. The
infection is particularly important in Italy and other parts of
Southern Europe, the middle east, parts of Africa and S.America,
and Taiwan, where the virus is endemic. Delta infection is
associated with both acute and chronic hepatitis, always in the
presence of hepatitis B, and superinfection in a HBV carrier can
lead to exacerbation of severe hepatitis. The damage caused by
the delta agent is probably due to a direct cytopathic effect of
the virus, in contrast to HBV where the damage is thought to be
immunologically mediated.
EPIDEMIOLOGY
The virus exists throughout the world and infection is always associated with serum that is positive for HBsAg. The presence of anti-Delta antibody in a subject who is negative for HBsAg but positive for anti-HBs indicates a previous infection. The infection is endemic in Southern Europe, Africa, the Middle East and, probably, Latin America. Delta is present in most of the countries of the world where it has been looked for, the one possible exception being China and Japan. Most of the countries of the Far East at the moment appears to have quite a low incidence of Delta with the exception of Taiwan. In Taiwan, it was reported that 26% of all acute hepatitis cases have Delta antigen in the serum. Similarly in India where 14% of all acute cases are reported positive for Delta antigen.
The transmission of the Delta agent mirrors that of HBV, being primarily parenterally transmitted. Sexual transmission appears to be less efficient mode of transmission as there is a lower incidence of Delta infection in homosexuals compared to IV drug abusers. "Clustering" occurs within families, the spread within families appear to be horizontal rather than vertical. Although vertical transmission can occur, it does not appear to be an important means of transmission.
The infection is observed particularly frequently among drug addicts, who are repeatably exposed to inoculation with HBV infected blood. This epidemiological category is currently responsible for the spread of virus into Northern Europe and the USA eg. In Sweden, there was no trace of Delta infection before 1973 but since then, the annual incidence amongst HBsAg positive drug addicts have progressively increased, reaching a rate of 72% in 1981. There is also a significant risk of infection in haemophiliacs who receive commercial factor VIII concentrates. Approximately 50% of these patients appear to contract the infection and develops liver disease. In the US, Delta infection was found in 20 - 53% of IV drug abusers, 40 - 80% of haemophiliacs, and 8 - 20% of homosexuals and dialysis patients who are known HBsAg carriers.
IMMUNOLOGICAL_ASPECTS_OF_DELTA_INFECTION
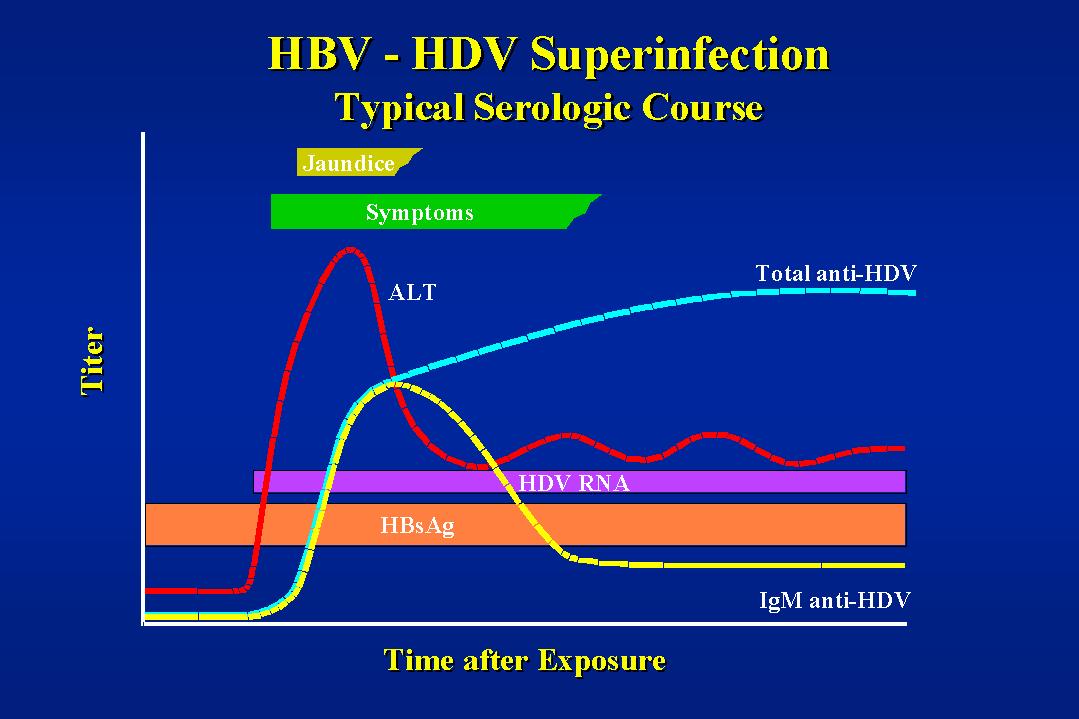
Against the background of an HBV infection, the initial stage of Delta infection is marked by the appearance of the Delta antigen in the liver, this is quickly followed by a phase where the Delta antigen is present in the blood, usually for a brief period and at pre-clinical levels. Consequently, in most cases, Delta antigen is not detected in the blood. The extent of the antibody response against the Delta agent depends on the extent and duration of the presence of Delta anigen in the blood. therefore, in a normally short acute coinfection, the response is usually limited to a brief appearance of anti-Delta IgM and a low, sometimes undetectable titre of IgG. If the infection is sustained, as in most cases of superinfection, the appearance of Delta IgM is followed by high titres of Delta IgG.
If the infection is resolved, then the Delta antigen in the
liver as well as the serum is eliminated. Delta-IgG, when it is
present, is the only sign of former infection. If the infection
becomes chronic, as is very likely in the case of superinfection,
the Delta antigen will persists in the liver whilst it will be
rapidly eliminated from the serum. Delta IgG should persists at
high levels, Delta IgM will also persists for a longer period of
time than acute infection. In practice, the Delta
antigen/antiboby system behaves in a similar way to the core
antigen/antibody system of Hepatitis B.
CLINICAL_ASPECTS
Coinfection with HBV is necessary for the Delta agent. Those who are immune to hepatitis through vaccination or natural infection will also be immune to HDV. Infection may occur in 2 ways :-
1. Coinfection with HBV of a patient not previously exposed to HBV.
2. Superinfection of a HBV carrier.
1._Coinfection
In the case of coinfection, the synthesis of the defective virus must necessarily follow the appearance in the circulation of the HBsAg induced by the coinfecting HBV. Hence one may see more than one rise in liver transaminase and there may be 2 peaks of ALT, although not always. The synthesis of the Delta agent cannot continue after the elimination of HBsAg. The clinical appearance is that of normal hepatitis B. Delta antigen is rarely detected in the serum, though anti-Delta IgM is found in the serum and lasts 2 - 6 weeks. Anti-Delta IgG may be present in a low level or perhaps not detectable at all. In general, the clinical course of acute hepatitis B is more severe in the presence of Delta coinfection. There is a much increased likelihood of developing fulminant hepatitis.
2._Superinfection
The most common form of Delta infection is superinfection of a known HBsAg carrier and it is where Delta infection produces its most deleterious effects. Preexisting HBsAg in the circulation captures the Delta virus, even if it is in small amounts and intensifies its synthesis immediately. Delta infection of a previously healthy carrier may induce an acute hepatitic picture. Infection in a carrier with preexisting hepatitis will aggravate the clinical picture.
Primary Delta infection in a HBsAg carrier is often severe, with a significantly higher number of fulminant hepatitis cases. The most serious aspect of superinfection by Delta is its tendency to become chronic and for the acute hepatitis to progress into chronic hepatitis (chronic active or persistent hepatitis and cirrhosis). At least 70 -90% of superinfected carriers develop chronic infection. (70% of such patients develop chronic active hepatitis, 20% cirrhosis and a minority chronic persistent hepatitis). In an outbreak in Venezuela, there was a 23% mortality rate and 80% of survivors went on rapidly to develop chronic active hepatitis and to cirrhosis. In an Italian study, where the progression rate of acute HBV to chronic active hepatitis without Delta is 1 - 2%, it was 2.4% in coinfections and 91% in superinfections. The rapid evolution of chronic hepatitis Delta may explain the rare occurrence of Delta markers in patients of hepatocellular carcinoma.
Delta superinfection in a HBsAg carrier should induce a quick
rise in liver enzymes. Delta antigen appears in the serum
followed by Delta IgM and Delta IgG. In contrast to acute
coinfection, Delta IgG can reach very high levels. Acute Delta
superinfection is accompanied by a drop in HBsAg in the HBV
carrier, sometimes to undetectable levels so that true diagnosis
could be masked. The serum picture remains the same whether the
infection becomes chronic or not. However, in the case of the
infection becoming chronic, Delta antigen persists in the liver
and can be detected by immmunoperoxidase or immunofluorescence
staining techniques.
DIAGNOSIS
1. Detection of Delta Ag in the liver - Liver biopsy specimens may be stained for Delta Ag by immunofluorescence or immunoperoxidase techniques. This method is particularly useful in the diagnosis of chronic Delta infection.
2. Detection of Delta virus RNA - the detection and quantitation of delta virus RNA by Real time qPCR or equivalent assays has been found to be of use in the management of infected patients.
3. Serology - Serum Delta Ag, anti-Delta IgM,
anti-Delta IgG or Total anti-Delta may be determined by
competitive or antibody capture radioimmunoassays. The results
must be interpreted in context with the HBV serology results :-
Anti-HBc Anti-Delta
HBsAg Total IgM HBeAg Anti-HBe Total IgM Anti-HBs
1. + + + + - + + -
2. + + - +or- +or- + + -
3. + + - +or- +or- + - -
4. - + - - + + - -
5. - + - - +or- + - +
1. Acute coinfection with HBV and Delta. (Probably cure).
2. Acute Delta superinfection (anti-Delta low), or chronic Delta superinfection (anti-Delta low).
3. Recovery from acute Delta superinfection (anti-Delta low), or, rarely, chronic Delta superinfection (anti-Delta level high), usually without symptoms.
4. Previous HBV and Delta infection with probable recovery.
5. Recovery from HBV and Delta infection.
The Delta antigen appears in the serum before or early in the course of clinical illness (a few days to a month or so), and thus it is often missed. However, if it is detected, it would indicate an acute attack. (One case has been reported where there is persistent Delta Ag in the serum. The patient concerned is a IV drug abuser who is also HIV positive.) It is recommended that the following should be tested for Delta infection :-
1. All drug abusers with jaundice, whether or not HBsAg positive, because of possibility of suppression of surface antigen.
2. All HBsAg positives (perhaps this is the easiest thing to do from an administrative standpoint.)
3. HBsAg carriers with chronic liver disease.
4. All fulminant hepatitis even if HBsAg negative.
MANAGEMENT
There is no therapy available at present against Delta. However, if HBV can be eliminated and thus HBsAg eliminated from the serum, Delta infection should then be eradicated. Interferon therapy of existing eAg +ve carriers may prove to be of value. However, since the replication of HBV is decreased by interferon, there would be less interference with Delta virus replication and thus Delta agent synthesis may well be increased initially giving a sudden deterioration in clinical disease.
In general, infection by HDV carries a poorer
prognosis than HBV disease alone and is associated with a higher
incidence of fulminant hepatitis, chronic hepatitis, and
cirrhosis. moreover, both infections together are likely to
spread within closed populations. In acute HBV/HDV coinfection,
the course of the illness is often self-limited. However, the
likelihood of developing chronic hepatitis is greater.
Superinfection with HDV can cause fulminant hepatitis and
establish a chronic HDV infection, possibly manifesting as
chronic active hepatitis and cirrhosis. In one study involving
192 chronic carriers in Los Angeles, CAH or cirrhosis was found
in 94% of patients who were HDV positive, compared to 61% of
patients who were HDV negative. Fulminant HDV hepatitis carried a
mortality rate of 70%. Prophylaxis against Delta infection can be
achieved by specific vaccination against HBV.
CDC
hepatitis branch; "Epidemiology and Prevention of Hepatitis
A-E: An Overview"