 |
 |
Pathogenesis of Rabies Infection
C. Pathogenesis
The commonest mode of transmission in man is by the bite of a
rabid animal or the contamination of scratch wounds by virus-
infected saliva. However, other routes have been implicated in
the past, such as through mucous membranes of the mouth,
conjunctiva, anus and genitalia. Infection by aerosol
transmission had been demonstrated in experimental animals and
has been implicated in human infection in rabies-infected bat
caverns and in several laboratory accidents. Man to man
transmission by transplantation of infected corneas were reported
in 5 instances. Rabies is an acute infection of the CNS which is
almost invariably fatal. The virus is similar to VSV of cattle.
Following inoculation, the virus replicates in the striated or
connective tissue at the site of inoculation and enters the
peripheral nerves through the neuromuscular junction. It then
spreads to the CNS in the endoneurium of the Schwann cells.
Terminally, there is widespread CNS involvement but few neurons
infected with the virus show structural abnormalities. The nature
of the profound disorder is still not understood.
D. Clinical Features
The incubation period is highly variable, ranging from 7 days to several years. It depends on several factors such as;
1. Dose of inoculum
2. The severity of the wound
3. The length of the neural path from the wound to the brain e.g. wounds on the face have a shorter incubation period than wounds in the leg.
The illness begins with a non-specific prodrome period, comprising of fever, malaise, anorexia, N+V, sore throat, myalgia and headache. The patient nay exhibit irritability and abnormal sensations around the wound. The prodrome is followed by one of two basic clinical patterns: the more common "furious" form characterized by hyperexcitability, spasms and hydrophobia; or "dumb" rabies featuring an ascending paralysis. Survival tends to be longer for patients with "dumb" rabies than those with "furious" rabies.
Complications involving the Cardiovacular System, CNS, and the
respiratory systems eventually develop and contribute to death.
Cardiac dysrhythmias of all types occur and respiratory
disturbances occur in all cases. Raised intracranial pressure
contributes to the decreased level of consciousness and to focal
convulsions. Other CNS complications include disturbances of
thermoregulation, diabetes insipidus, autonomic dysfunction and
convulsions. The differential diagnosis of rabies includes
tetanus, poliomyelitis, Guillain-Barre syndrome, viral
encephalitis and poisonings and drugs.
E. Laboratory Diagnosis
The diagnosis of animal and human rabies can be made by 4 methods: (1) histopathology (2) virus cultivation (3) Serology (4) virus antigen detection. Although each of the first 3 methods have distinct advantages, none provide a rapid definitive diagnosis.
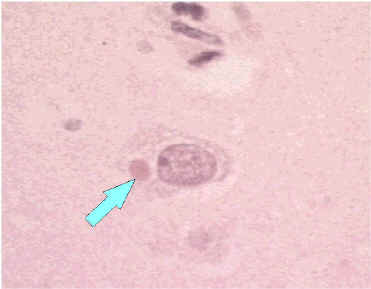
Negri body in body of neuron and positive IF test for rabies antigen (Source: CDC)
F. Management and Prevention
Once rabies is established, there is nothing much that could be done except intensive supportive care. To date, only 2 persons with proven rabies have survived, and 3 persons with probable rabies. However, one survivor was left with severe neurological sequelae and all 3 who recovered were vaccinated beforehand. Numerous antiviral agents have been tried with no success.
1. Postexposure prophylaxis
In cases of animal bites, dogs and cats in a rabies endemic area should beheld for 10 days for observation. If signs develop, they should be killed and their tissue examined in the laboratory. Wild animals are not observed but if captured, the animal should be killed and examined. The essential components of postexposure prophylaxis are the local treatment of wounds and active and passive immunization.
2. Preexposure prophylaxis
Persons who are regularly at high risk of exposure, such as vets, laboratory workers, animal handlers and wildlife officers should be considered for preexposure prophylaxis by active immunization with the cell culture vaccine. Immunization normally consists of 3 doses of vaccine. Antibody can be demonstrated in the sera of virtually 100% of those vaccinated if the diploid cell culture vaccine is used. Booster doses should be offered to persons at continuing risk every one to three years. Local treatment of wounds should always be carried out in exposed persons who have been vaccinated previously. The WHO expert committee considers that local infiltration with antiserum is optional and systemic passive immunization contraindicated.
3. Rabies Vaccines
Several types of live attenuated vaccines are available for use in animals, but they are considered to be unsuitable for humans. The vaccines which are available for humans are present are inactivated whole virus vaccines.
Another inactivated vaccine is widely used in China. It is derived from virus grown in primary hamster kidney cells and cost less than the other diploid cell culture vaccines. The vaccine had been shown to be as effective as HDCV. Efforts are being made to use other inexpensive cell culture systems such as VERO cells.
4. Failure of prophylaxis
HDCV has been used to treat many thousands of people exposed to possible rabid animals in the past 12 years and its efficacy has been proven. At least 16 people treated with HDCV after exposure have died of rabies. All of the patients had major exposures and in the majority, the incubation period was short, 21 days or less. Treatment was frequently not started promptly within 24 hours and only half received combined serum and vaccine. At least one person has died despite optimum treatment.
G. Rabies Control
Urban - canine rabies accounts for more than 99% of all human rabies cases and over 90% of all human post-exposure treatments worldwide. In the past, the Scandinavian countries were able to rid themselves of rabies by sanitary control alone, which included stray dog control. Other countries, such as the UK, have used these techniques allied with quarantine and/or vaccination to eradicate and then maintain freedom from the disease. Currently, the importation of mammals into the UK is controlled by the Rabies order. It applies to a wide range of mammals but livestock including horses, which are covered by separate regulations. The animals must be vaccinated on arrival. Effective animal vaccines are available.
Wildlife - canine rabies can be controlled because in general, dogs live in close association with man and are therefore within physical reach. An attempt was made to vaccinate foxes in an attempt to create an immune barrier at the entrance to the Rhone valley in 1978. The live attenuated virus was contained in small plastic blister packages fixed under the skin of chicken heads used as a bait, and 4050 of these were distributed over an area of 335km2. With continued field trials, Switzerland has been freed of rabies. Other field trials are being set up.