Epidemiology of Varicella Zoster Virus Infections
C. Epidemiology
Primary varicella is an endemic disease. Cases of varicella
are seen throughout the year but, like other viruses spread by
the respiratory route eg. measles and rubella, they are seen more
commonly in the winter and early spring. This is unlike that for
enteroviruses and lends some support to the view that varicella
is spread mainly by the respiratory route. Herpes zoster, in
contrast, occurs sporadically and evenly throughout the year.
Varicella is one of the classic diseases of childhood, with the
highest prevalence occurring in the 4 - 10 years old age group.
Like rubella, infection is uncommon in preschool children.
Varicella is highly communicable, with an attack rate of 90% in
close contacts. Most people become infected before adulthood but
10% of young adults remain susceptible. However, this pattern of
infection is not universal, eg. in rural India, varicella is
predominantly a disease of adults, the mean age of infection
being 23.4 years. It was suggested that this could be due to
interference by other respiratory viruses that the children are
exposed to at an early age.
D. Clinical Features
I. Varicella
1. Symptoms and Signs
The incubation period is 7 - 23 days (mean = 2 weeks). A
shortened incubation period can be especially encountered in
immunocompromised patients. In children, the illness begins with
the characteristic rash but in adults, a prodrome resembling an
influenza-like illness commonly presents a few days earlier. Neck
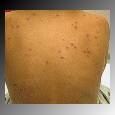
lymphadenopathy is commonly present. The rash is
characteristically centripedal in distribution and is seen mainly
in areas not exposed to pressure, such as the flank, shoulder
blades, and in the axillae. The skin lesions progress rapidly
through the stages of macules to papules to vesicles which
rapidly break down with crust formation. The lesions appear in a
series of crops so that all stages in their genesis can be seen
at any one time. Patients with varicella are generally considered
to be infectious 2 days before the appearance of the rash and 7
days after onset, when the vesicles have crusted.
The disseminated vesicular rash of chickenpox
2. Complications
3. Immunocompromised individuals
Acute varicella infection is most serious in immunocompromised patients, in particular children with leukaemia, or receiving renal allografts. Without antiviral therapy, 30% of children with acute leukaemia who contracted varicella developed pneumonitis and 10% of them died. Thus the prevention of VZV infection is a high priority in such patients.
4. Varicella in pregnancy
Approximately 10% of women of childbearing age are still susceptible to varicella. Varicella is thought to occur 1 in 10,000, or 0.01% of all pregnancies. Varicella can cause problems if it occurs early or very late in the pregnancy.
1. Early pregnancy - maternal varicella rarely cross the placenta to cause congenital defects. However, occasionally it can cause a range of congenital defects similar to the congenital rubella syndrome. This is referred to as the "congenital varicella syndrome". With all these cases, maternal infection occurred before 20 weeks of pregnancy. There are at least 8 reports of infants with defects suggestive of congenital varicella syndrome whose mothers had herpes zoster during the first 4 months of pregnancy. However, in no case was there laboratory evidence of intrauterine infection with VZV and thus the association could be coincidental. There are at present inadequate data to provide an accurate assessment of the risk of congenital infection. It is undoubtedly a very rare complication of maternal varicella. The actual risk of transplacental infection in the first trimester is certainly less than 3%. The diagnosis of congenital varicella can be confirmed in many cases by the detection of IgM at birth. The nature and distribution of the lesions suggests that they are caused by reactivation of the virus in utero rather than by primary infection.
There are now at least 25 reports of children who developed zoster with no previous history of chickenpox. The mothers of these infants had chickenpox whilst they were 3 to 7 months pregnant. It was postulated that these infants were infected in utero at a time when their immune systems were too immature to maintain latency. In general, case reports of zoster, whether resulting from pre- or post-natal infection, supports the hypothesis that the earlier the child gets chickenpox, the earlier it is likely to get zoster.
2. Varicella in the late stages of pregnancy - varicella can cross the placenta in the late stages of pregnancy, causing congenital infection of the fetus. Infection acquired in this way may result in the child developing varicella in the neonatal period. This type of infection is referred to as neonatal varicella. The actual risk of the child acquiring infection depends on;
- The rapidity of the mother developing humoral immunity and transferring it across the placenta.
- The time interval between the date of onset of the rash in the mother and the date of delivery. The critical period is 7 days; if the rash occurred more than 7 days before delivery, sufficient immunity will have been transferred so that even if congenital infection occurs, it is likely to be mild. Neonates are more likely to experience severe disseminated disease if the maternal rash occurred 7 or fewer days before delivery.
Babies born to seronegative mothers who are infected in the perinatal period are also likely to experience severe infection as they do not have protection of VZV specific maternal IgG. Most neonates with congenitally acquired infection or otherwise cope remarkably well. Earlier reports of a fatality rate of 30% are definitely exaggerated.
II. Herpes Zoster
1. Symptoms and signs
Herpes Zoster mainly affects a single dermatome of the skin. It may occur at any age but the vast majority of patients are more than 50 years of age. The latent virus reactivates in a sensory ganglion and tracks down the sensory nerve to the appropriate segment. The lower cervical, thoracic and lumbar posterior root ganglia are most commonly involved. The eruption is commonly preceded by paresthesia, burning pains and tenderness of the skin. The trigeminal ganglion is another common site of reactivation and the ophthalmic branch of this nerve is 20 times more likely to be involved than the 2 other branches. The sacral ganglia may be involved where it may be associated with retention of urine or sometimes frank haemorrhagic cystitis. Facial palsy associated with vesicles in the external auditory meatus is known as the Ramsay-Hunt syndrome and is thought to be a form a zoster involving the VIIth nerve. It is often accompanied by hearing loss and vertigo. Herpes zoster has also been implicated as a cause of Bell's palsy without vesicles.
As with varicella, herpes zoster in a far greater problem in
immunocompromised patients in whom the reactivation occurs
earlier in life and second attacks, which are virtually unknown
in the immunocompetent, are frequently seen. The disease process
is likely to be prolonged in the immunocompromised individual and
the disseminated form is more likely to be present.
An example of shingles
2. Complications of Herpes Zoster
E. Laboratory Diagnosis
The clinical presentations of varicella or zoster are so characteristic that laboratory confirmation is rarely required. Laboratory diagnosis is required only for atypical presentations, particularly in the immunocompromised, and for distinguishing between HSV infection and herpes zoster.
1. Direct Methods
B. Virus isolation
This remains the definitive method for diagnosing VZV infections. Human fibroblasts are used in most laboratories. Vesicle fluid and scrapings form the base of fresh lesions are the most suitable specimens. Virus can rarely be recovered from crusted lesions. Biopsy material can also be cultured. The CPE produced by VZV is so characteristic that most laboratories do not undertake further identification of the isolates. Immunofluorescence of the cell sheet by monoclonal antibodies is the method of choice for identification. Virus isolation for VZV is rarely carried out because of the long length of time required for a result to be available.
Cytopathic effect caused by VZV in cell culture. (Courtesy of Linda Stannard, University of Cape Town, S.A.)
3. Serology
The most important use for serology is the determination of immune status before the administration of prophylactic therapy. Serological diagnosis of primary varicella infection can be reliably carried out using paired acute and convalescent sera. However, this is less reliable in the case of herpes zoster where there is specific antibodies present already. Therefore it is essential to obtain the first sample as soon as possible after the onset of the rash in order to demonstrate a rising titre. The sharing of antigens between HSV and VZV can make the interpretation of results very difficult. Where possible, the serological diagnosis should be backed up by virus isolation.
F. Management
1._Varicella
Varicella is normally a mild disease in immunocompetent individuals and no specific treatment is normally required. Varicella in immunocompromised patients can be a serious and potentially fatal disease. Due consideration must be given to the reduction or withdrawal of any immunosuppressive therapy and the administration of antiviral chemotherapy. Acyclovir is now the drug of choice (VZV is not as susceptible to acyclovir as is HSV and requires 10 fold higher concentration of the drug for effective inhibition) for the treatment of varicella in the immunocompromised and also in normal patients with VZV pneumonia. Approval has also been given in the US for the use of acyclovir for the treatment of chickenpox in otherwise healthy children and adolescents. A multicentre trial of acyclovir demonstrated the efficacy of acyclovir in accelerating cutaneous healing, reduced fever and constitutional symptoms. The use of acyclovir in such an instance is highly debatable and should be left to the primary care physician with full knowledge of the medical and economic factors. Acyclovir is also being increasingly used for prophylactic purposes in immunocompromised patients but it is not possible to give guidelines on their use at present. Other drugs are being evaluated at present. A compound known as 882C had specific activity against VZV but without any significant activity against HSV or CMV. Specificity is achieved by the requirement of the drug for VZV thymidine kinase in order to be converted to the monophosphate and the diphosphate form.
2. Herpes Zoster
herpes zoster in a healthy individual is not normally a cause for concern. The main problem is the management of the postherpetic neuralgia. Most modern analgesics are ineffective and opiates should not be given for prolonged periods. Steroids have been reported to be effective but should be given carefully because of the immunosuppressive nature of the drug. Heroic surgery involving the removal of the dorsal roots may be required for those with severe intractable pain. More severe forms of zoster, particularly disseminated disease, are seen in immunocompromised individuals. In contrast to primary infection, reactivation rarely results in life-threatening infection with visceral involvement in these patients. Nevertheless, antiviral chemotherapy is increasingly being given in order to reduce the risk of dissemination and the duration of the illness.
Acyclovir is the drug of choice and studies have shown that it
reduces the duration of virus shedding and accelerates healing
but should be given within 48 hours of the onset of symptoms.
Acyclovir is usually not justifiable in individuals without
underlying disease, except perhaps in the case of ophthalmic
zoster when it can be given orally to reduce the risk of ocular
complications. The treatment should be continued for 7 days.
Previously, it was thought that acyclovir has no effect on
zoster-associated but more recent studies suggest that it may be
particularly beneficial to those over 50 years of age. Following
treatment with the recommended dose of acyclovir (800 mg 5 times
daily), these patients become pain-free twice as fast as those
receiving placebo. The International Herpes Management Forum now
recommends that antiviral therapy should be offered routinely to
all patients over 50 years of age presenting with herpes zoster.
The advent of newer agents such as valaciclovir and famciclovir
will expand the range of antiviral therapies available to the
practitioner. In an intent-to-treat analysis of all patients
treated within 72 hours of rash onset, famciclovir, the oral
pro-drug of penciclovir offered no advantage over acyclovir.
However, valaciclovir was reported to resolve zoster-associated
pain about one-third faster than acyclovir. There had been no
published comparative studies of valaciclovir and famciclovir.
G. Prevention
Preventive measures should be considered in individuals at risk of serious disseminated varicella infection ie. the immunocompromised and neonates. Immunocompromised individuals should be advised to avoid contact with people with varicella or zoster. If contact has been made, prophylaxis with passive immunization or antiviral chemotherapy should be considered.
1. Passive Immunization
Zoster immune globulin (ZIG) were prepared from patients recovering from shingles. Now ZIG is prepared from blood donors with high titres of anti-VZV. ZIG ii frequently in short supply and if unavailable, prophylactic acyclovir or HNIG should be given. A reasonable history of varicella from a contact is a reasonable indicator of immunity and obviates the need to administer any prophylactic. Nevertheless, definitive assessment of the immune status can only be made on serological testing. In any case, the administration of ZIG should not be delayed until the results are available although a baseline sample should be obtained. ZIG is not totally effective in preventing infection by VZV. In a study carried out in the UK, 18 out of 27 (67%) seronegative children given ZIG were infected (compared to a normal infection rate of 90%), 14 of whom had symptoms. The rationale of administering ZIG to those at risk is not so much to prevent infection but to prevent the more serious forms of illness with visceral involvement. The actual effectiveness of ZIG in attenuating varicella has yet to be established fully by clinical trials. It is important, particularly in a hospital environment, to bear in mind the shortcomings of ZIG as patients given ZIG are still liable to develop varicella and become a source of infection to others.
ZIG should also be given to susceptible pregnant women in close contact with VZV infection in the hope that it will reduce the risk of transmission to the fetus. Again there is no data on the actual efficacy. In any case, VZV infection is likely to be more severe in pregnant women. ZIG should also be given to the newborn infants of mothers who contract varicella perinatally. It should be noted that acyclovir is not licensed for use in pregnant women or neonates. The types of patients at risk of contracting the severe forms of varicella are listed below ;-
2. Active Immunization
The currently marketed varicella vaccines are based on the Oka strain of VZV which originated from Japan. It has been modified through sequential propagation in different human and animal cell cultures. Various formulations of such live, attenuated vaccines have been tested extensively and are approved for use in Japan, the Republic of Korea, the United States and several countries in Europe. Some formulations are approved for use at 9 months of age and older. Following a single dose of the above-mentioned vaccines, seroconversion is seen in about 95% of healthy children. From a logistic as well as an epidemiological point of view, the optimal age for varicella vaccination is 12-24 months. In Japan and several other countries 1 dose of the vaccine is considered sufficient, regardless of age. In the United States, 2 doses, 4-8 weeks apart, are recommended for adolescents and adults, in whom 78% were found to have seroconverted after the first, and 99% after the second dose of the vaccine. Children below 13 years receive only 1 dose. Small studies, using formulations different to that currently licensed in the US, show that when the vaccine is administered within 3 days after exposure to VZV, a postexposure protective efficacy of at least 90% may be expected. Varicella in persons who have received the vaccine ("break-through varicella") is substantially less severe than the disease in unvaccinated individuals. Further studies are needed to clarify the postexposure efficacy of the currently licensed product, especially in outbreak situations.
Live attenuated vaccines are normally contraindicated in immunocompromized individuals. Clinical trials showed that in normal symptomless individuals, symptomless seroconversion is regularly achieved in up to 90% of the vacinees, but the levels of antibodies are substantially lower than observed after wild virus infection. The seroconversion rate is lower in immunocompromized patients. The vaccine also confers significant protection in immunocompromised children but can cause mild symptoms of rash and fever. The vaccine strain is sensitive to acyclovir should that be required. The vaccine is potentially useful for postexposure prophylaxis. Antibody responses do not appear 3 to 5 weeks after vaccination but CMI responses develop within 4 days of vaccination in approximately 50% of vaccinees and has been shown to confer protection shortly after contact. On the downside though, the vaccine can establish latent infection in some vacinees and reactivate to cause zoster. However, this occurs far less often than the wild-type virus. The vaccine is transmissible and when it is transmitted, it causes a mild rash in most cases. The prime target for vaccination will be young seronegative children who are immunocompromised. Consideration is also being given to the possibility of vaccinating seropositive adults with the aim of preventing zoster. In the US, the vaccine has now been licensed and is part of the routine universal vaccination programme in children. A single dose of vaccine is given at 12 months of age. For older children and adults over the age of 12, two doses of vaccine are required. Cost benefit analyses which had been carried out were in favour of universal vaccination, especially taking into account the time that parents may have to take off from work as a result of their child’s illness.
In the past, certain lots of the vaccine given to leukaemic children on maintenance chemotherapy resulted in a high incidence of vaccine-associated chickenpox which was sometimes severe. Fortunately, there were no deaths and the lots which were identified contained less-attenuated virus. The newer lots in use appears to be very safe. The prime target for vaccination will be young seronegative children who are immunocompromised. Consideration is also being given to the possibility of vaccinating seropositive adults with the aim of preventing zoster. In view of the efficacy of ZIG and acyclovir in preventing and treating chickenpox in immunocompromized children, caution should be exercised before the vaccine is recommended for immunocompromized children. However, the following criteria should be considered for vaccination.
At St Bartholomew’s hospital, UK, 50 leukaemic patients have been vaccinated with a seroconversion rate of 70%. It has been proved to be a safe and effective vaccine. 1 booster dose should be given. The breakthrough infection rate is less than 10% after close contact. The vaccine elicit rapid efficient CMI and can thus be used in postexposure prophylaxis. The problem with this vaccine is that it can remain latent and reactivations can occur, However, reactivations tend to be less serious. The vaccine is expensive to produce and is relatively unstable, requiring storage at -20oC.
As in the case of mumps, there is a lot of controversy as to whether VZV should be incorporated as part of a universal vaccination program. Several cost-benefit studies had been carried out in different countries which claim to show a benefit. In theory, it should be possible to incorporate VZV into the current MMR vaccine which will increase its attractiveness. At present though, it is still up to the parents to decide whether to vaccinate their children or not. The cost of the vaccine is borne by the parents in most instances.
3. Management of outbreaks in hospital
Patients with uncomplicated chickenpox do not require
admission to hospital. If admission is required, then the patient
should be put in respiratory isolation. The same applies to
patients with other conditions who develop chickenpox while in
hospital. For patients with shingles, contact isolation would be
sufficient. Other patients on the ward should be assessed for
immunity for VZV; usually, a past history of a chickenpox-like
illness diagnosed by the General Practitioner is sufficient;
however, IgG antibody screening of all patients would be
preferable, especially for those individuals who are predisposed
to severe chickenpox. Those found to be negative should be
discharged home if their condition allows. If they must remain in
hospital, they should be cohorted together and put in respiratory
isolation for at least 21 days until the incubation period has
passed. ZIG should be given to seronegative patients who are
susceptible to severe VZV disease such as leukaemic children,
immunocompromised individuals. These patients who are given ZIG
and isolated should be isolated for at least 28 days since ZIG is
known to prolong the incubation period. Likewise, staff should be
assessed for past immunity to VZV, if negative, they should
either refrain from work for 21 days (US guidelines), or remain
in the same ward, or transferred to other wards with
immunocompetent patients doing work which requires less patient
contact. With the availability of the vaccine, it may be
advisable to screen all staff in high risk wards and immunized if
found to be negative. The problem is whilst this is easy for
staff permanently based on the ward, there is also a high
turnover of non-permanent staff such as doctors, domestics,
porters etc. There is now active discussion on the possibility of
screening and administering the vaccine to medical and nursing
students.
H. VZV infection during pregnancy
Varicella is one of the classical diseases of childhood. The majority of individuals has been infected before reaching adulthood so that varicella is uncommon during pregnancy. The actual incidence of varicella during pregnancy is not known but is now thought to be more common than rubella because of rubella vaccination. Pregnant women who contract VZV are at risk for the more serious complications such as pneumonia and encephalitis, which may be fatal. There is controversy surrounding the administration of ZIG to susceptible women in contact with chickenpox. There is evidence to suggest that ZIG does reduce the attack rate and the severity of the disease and thus should be given to pregnant women if supplies permit. Intrauterine and perinatal infection may occur with three possible clinical expressions;-
1. Congenital varicella syndrome
Congenital varicella syndrome comprises of a number of abnormalities, some of which scarring of the skin and hypoplasia of one or more limbs are characteristic. Other abnormalities include CNS and eye abnormalities, abnormalities of the GI and GU tract. Death occurs in infancy in many cases. It had been postulated that the principal manifestations of varicella embropathy are not caused by primary infection of the fetus but by in utero reactivation of virus whose period of latency in the fetal nervous system has been shortened by immunological immaturity.
The incidence of embryopathy is difficult to determine. For a start, the syndrome is ill defined. Scarring of the skin and hypoplasia of a limb are characteristic but CNS and eye abnormalities may be due to other causes. The risk had been reported to be 3% but this is likely to be an over-estimate. There are at least eight case reports of infants suggestive of congenital infection born to mothers with a history of zoster during the first 4 months of pregnancy, however this association may be coincidental and to date, there is no firm data linking maternal zoster to congenital infection. Specific IgM can be detected from the cord blood in many, but not all cases of suspected congenital varicella syndrome.
2. Zoster in childhood
Cases of childhood zoster had been reported from infants whose mothers contracted chickenpox during the second and third trimester of pregnancy. Other cases of childhood zoster occurs in children who contracted chickenpox very early in life. In general, case reports of childhood zoster, whether resulting from pre or post-natal infection, supports the hypothesis that the earlier the child gets chickenpox, the earlier it is likely to get zoster because of the immaturity of the immune system.
3. Neonatal chickenpox
Chickenpox during the first few months of life is uncommon, partly because of the lack of exposure and because of the presence of maternal IgG. The newborn child of a non-immune mother may contract the disease if the mother develops the rash at the time of delivery. The severity of the disease may vary from a few spots to a severe fatal disease with pneumonia and general dissemination involving the lungs, spleen, heart, pancreas, kidneys and suprarenal glands. The fatality rate of 30% that had been reported is probably exaggerated. The risk of a child acquiring varicella is dependent on the rapidity with which the mother develops and transfers humoral immunity across the placenta and that depends on the time interval between the date of onset of the rash in the mother and the date of delivery. If the onset of the rash in the mother occurred seven days or more before delivery, sufficient immunity will have been transferred so that even if infection has occurred in utero, the infection will be mild or inapparent. Thus the period of high risk is the development of maternal rash between 5 days before delivery and 2 days after delivery. ZIG should be given to all infants whose mothers develop chickenpox during the last seven days of pregnancy or the first 14 days after delivery but its effect is uncertain. In all probability, it probably does reduce severity.